Work at a brand-new purpose-built residential care home for children has now started on site in Nuneaton, including four stand-alone residential care homes and associated facilities. The £5.1 million state-of-the-art build, named The Forge, has been designed to provide a safe, secure and encouraging place for up to 20 children who are experiencing emotional and behavioural disorders or recovering from early childhood trauma.
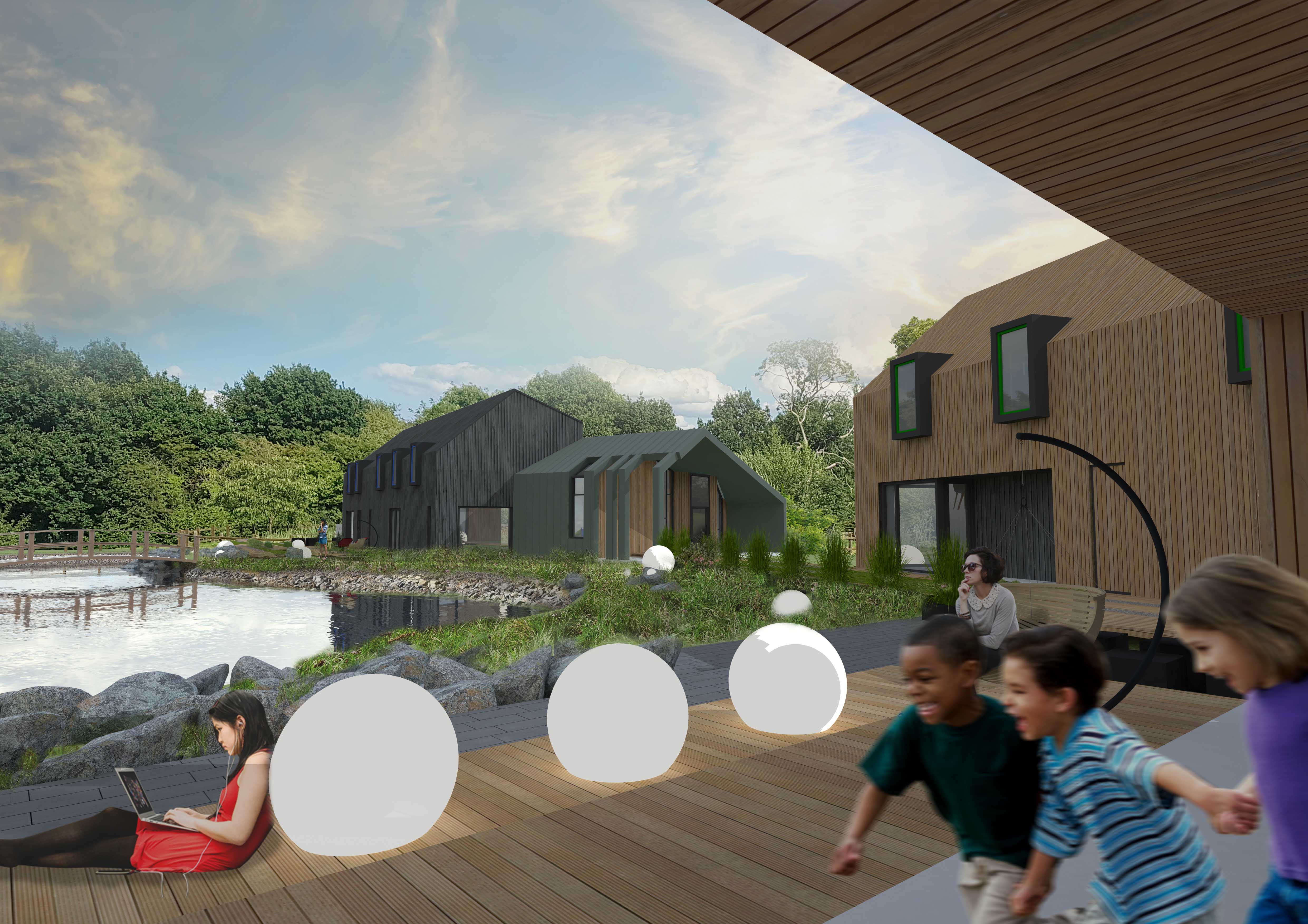
Located off Plough Hill Road, the therapeutic facility is being developed by Nuneaton based children’s home provider Forge Care, with Rugby-based construction partner Stepnell as the main contractor and Coventry-based architects IDP. Once complete, the ground-breaking scheme will provide more than 80 jobs on site for the local area and will become a flagship scheme for Forge Care, offering the highest level of care with a strong focus on quality spaces, materials and design principals.
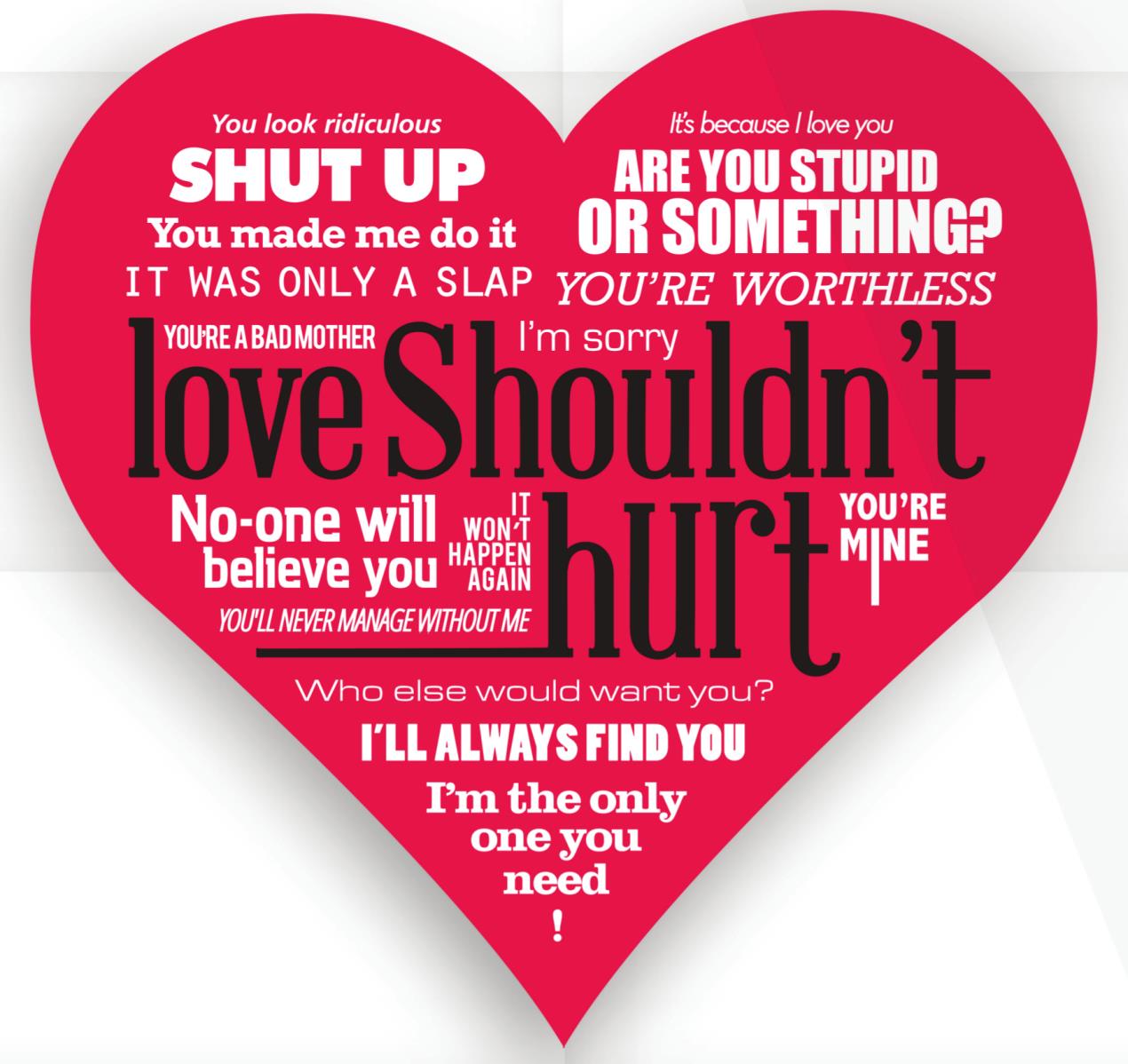
Gavin Miller, director at Forge Care, said: “We are excited to have this flagship project underway, The Forge is a trauma-informed service that evolves as a whole system underpinned by the Sanctuary Model. Within our Therapeutic Community environment the social relationships, structure of the day and activities are all deliberately designed to facilitate learning, and develop people’s personal, social health and wellbeing.
“It has been a pleasure working with our various suppliers, and keeping those suppliers local was an important factor in selecting our team, from our designers and architects to our building contractors, working with companies based in Warwickshire was important for us and we are proud of what we have achieved as a team.”
Regional director at Stepnell, Adrian Barnes, said: “We’re delighted to be starting on site at The Forge and we are incredibly proud to be involved in a project that will have such a big impact on the local community, particularly vulnerable children looking for a safe and secure place to call home. The scheme is ground-breaking in a number of ways and we are confident that it will have the ‘wow factor’ once finished.
“We are really excited to be on site and get started on this fantastic scheme, and we will be adhering to strict COVID-19 and Public Health England Guidelines throughout the build to ensure that we are keeping everyone safe.”
Each of the four individual buildings at The Forge will incorporate a welcome space, main lounge, kitchen, quiet space, games, and an activity space, as well as five en-suite bedrooms on the first floor, to replicate the traditional family home layout.
Marcus Jones MP said: "I am pleased to welcome a new, purpose-built, children's care home in Nuneaton. Sadly, some children need specialist care to overcome traumas that would otherwise blight their young lives. The team at Forge Care is committed to helping young people overcome the problems they have encountered and to realise their full potential. I wish the staff and residents at The Forge every success."
The development has a strong focus on sustainability, using carefully selected materials like timber cladding and zinc, and will provide a variety of green space to promote physical activity and wellbeing.The communal amenity space will include a games area and a stand-alone art room. Outside, children will have access to large play areas that support mental and physical health – such as yoga and meditation amenities - as well as external dining and BBQ’s for the warmer months.
The external spaces will also feature sensory and nature spaces, to encourage residents to grow plants or food and encourage wildlife, while utilising the existing pond to provide a tranquil setting for residents.
Jenny Bachelor, associate architect at IDP, said: “IDP is incredibly proud to have been involved with The Forge since early concept sketches and development of the brief. As a multi-disciplinary practice experienced in quality healthcare design our involvement has embodied architectural design and services, interior design, landscaping, technical delivery and cost consultancy, and we are very much excited to see the homes built as they were intended to be.
“It is such a unique and forward-thinking project in its care model and design and it is a real credit to Forge Care and the wider team that this has been made possible. The design encompasses a collection of four truly bespoke homes nestled within intimate gardens and individually designed to orientate outlook and maximise connectivity to the beautiful site, all in the interest of aiding recovery.
“Each en-suite bedroom also has its own window seat towards the main garden and a soft natural and monochrome finish has been used to offer a calming backdrop to the colourful interior design. The Forge seeks to provide a safe and nurturing environment very much in tune with the high level of care that will be provided there, yet its playfulness encourages a sense of adventure and intrigue.” As well as the four care homes, there will be 21 car parking spaces, including two disabled spaces and cycle parking for staff. The existing community building is remaining on site.
The development received planning approval from Nuneaton and Bedworth Borough Council in 2018 with funding finalised last year from Assez Capital. The residential development is expected to be completed by Christmas 2021.